Claim rejections from DrChrono's billing system, the clearinghouse, or the payer will be displayed in your Live Claims Feed (LCF) for review, correction, and resubmission.
Here's how to identify them:
- Hover over Billing and select Live Claims Feed.
-
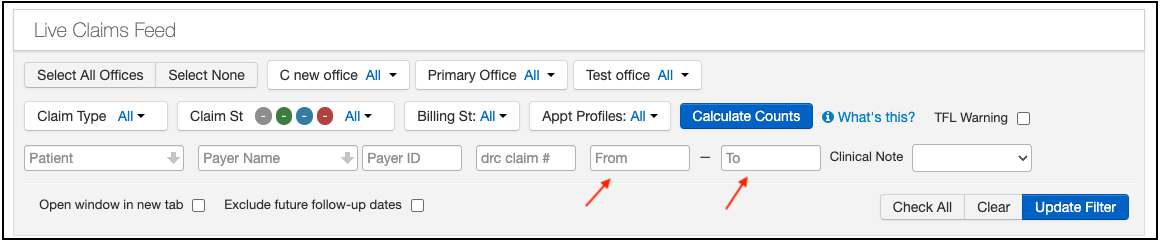
You will first want to update the date range to ensure you are capturing all claims. The system will default to the past month, but it can be changed by using the to and from date boxes.
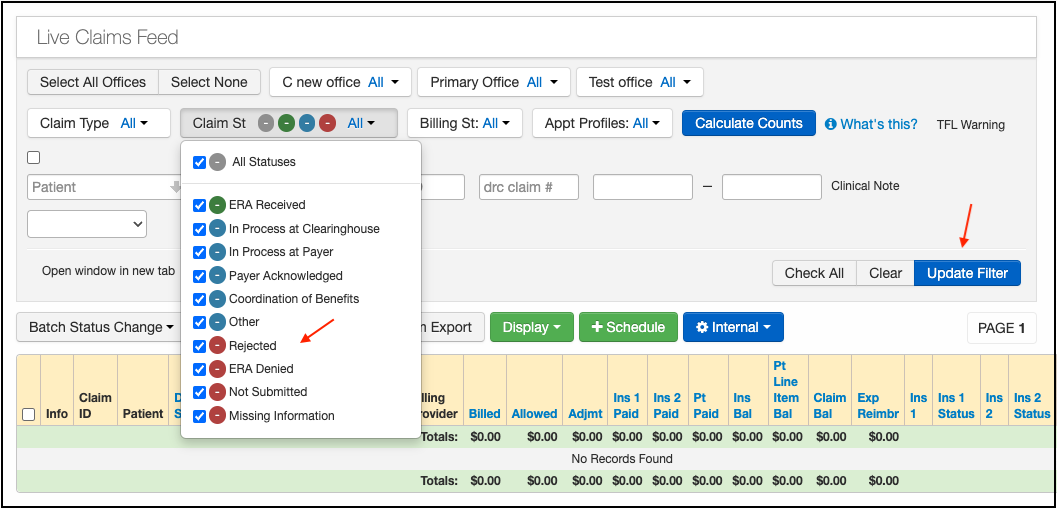
- Next, press the blue Calculate Counts in the middle of the screen. This will have the system count the number of claims you have in each status, making it easier to identify those that need attention.
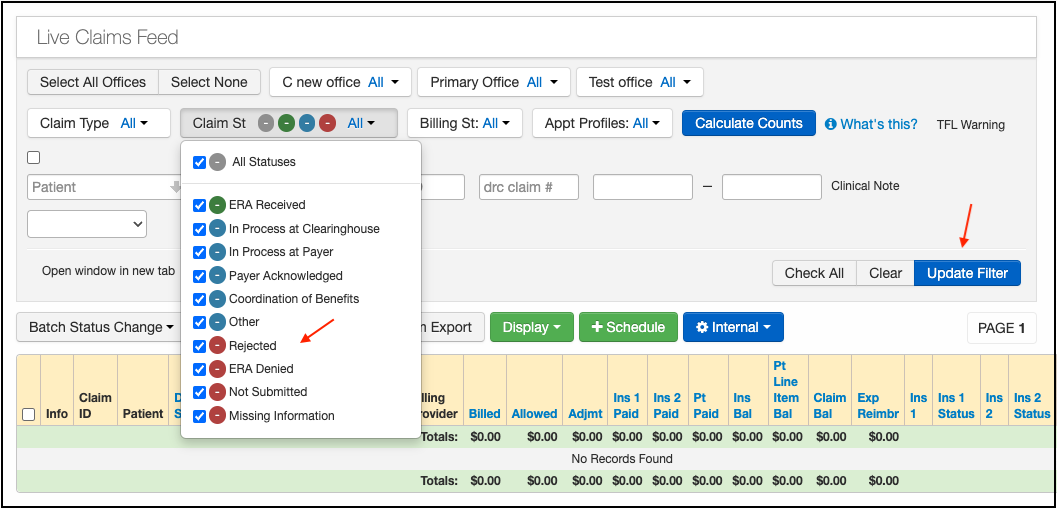
- Select the Claim St Dropdown, you will need to uncheck All Statuses and choose any (or all) of the 3 denial/rejected statues: Rejected, ERA Denied, or Missing Information.
- Press on Update Filter. The system will display the claims that match your status and date range parameters.
- Press the blue Date of service to go into the billing details screen.

- In the Billing Detail screen, press on the link that reads Rejected/Missing Information/ERA Denied.

This will display a pop-up window that will provide details of the rejection reason. Once the rejection reason is known, you will be able to make the appropriate corrections and resubmit the claim, if needed.
To resubmit the claim, just check the box Resubmit claim and then press Verify and Save.


The best practice is to review for denials each day. A claim that is sitting in one of these statuses is not being processed by a payer, which means that your reimbursement will be delayed.