Sometimes a payer will retract a payment from an appointment that was previously paid.
An example would be when the patient was not eligible on the date of service. They could have paid the claim with the information that the patient was active but subsequently received information (usually from their employer) that the patient was not eligible on the date of service. They audit their system and sometimes find where they have paid out on a claim they shouldn't have; thus the retraction.
If the retraction comes in on an ERA, it will be posted for you. The directions below will assist if you need to post it manually.
- Navigate to Billing > Live Claims Feed.
- Select the patient for whom the payment has been retracted and enter their billing details.
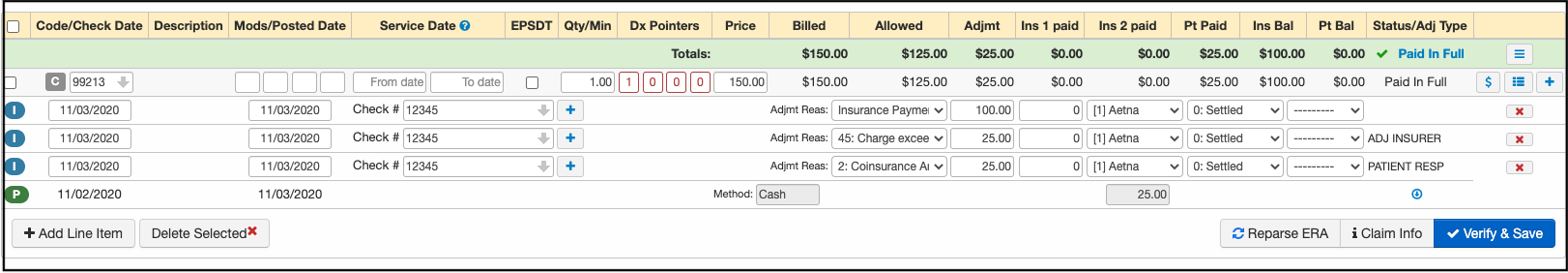
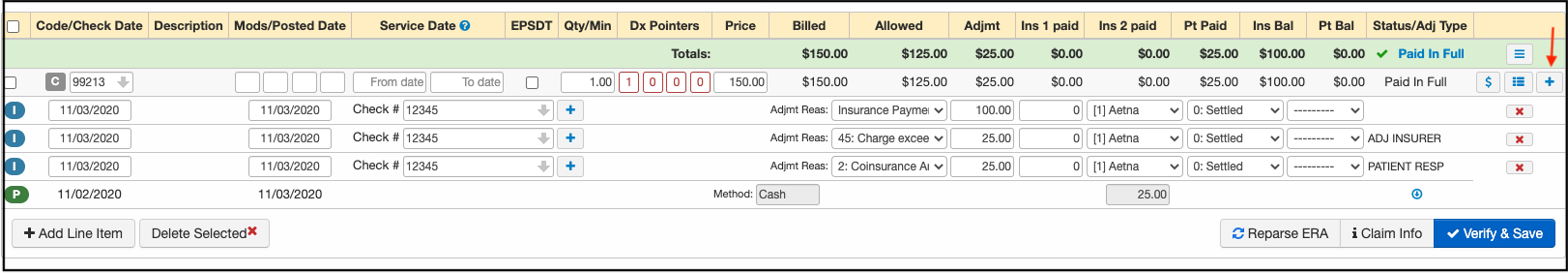
- Scroll down to the bottom where the payment is posted.
- Press on the blue + sign and add as many rows as you need (1 for Insurance Payment; 1 for contractual adjustment; 1 for copay, plus any additional that are listed on the EOB)
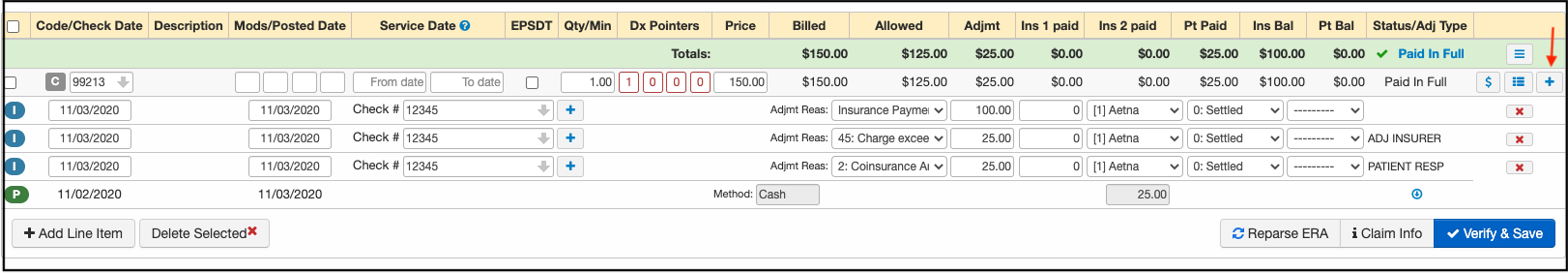
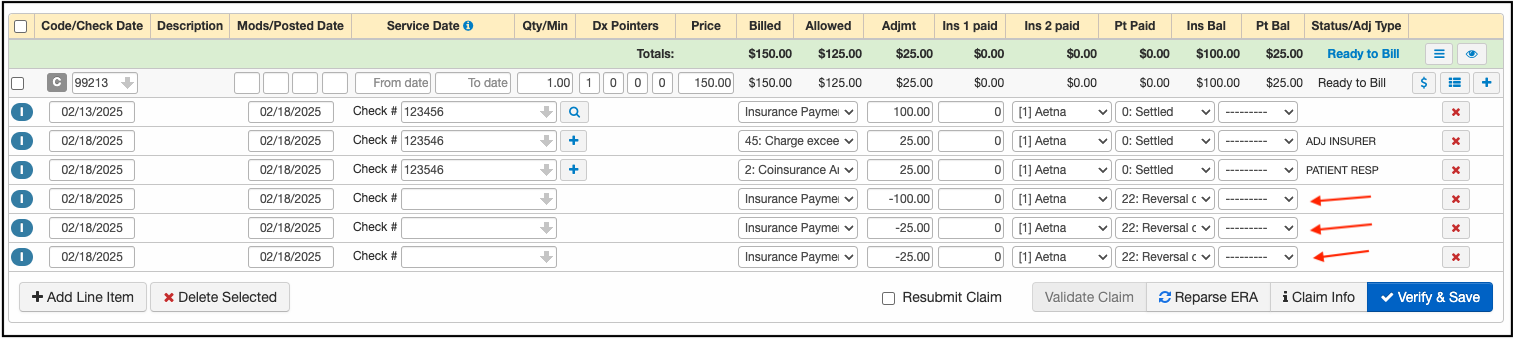
- Post the payment, contractual adjustment, and any patient responsibility as negative amounts using code 22 to designate it as a reversal of the previous payment. Posting negative amounts to each line item to reverse them.
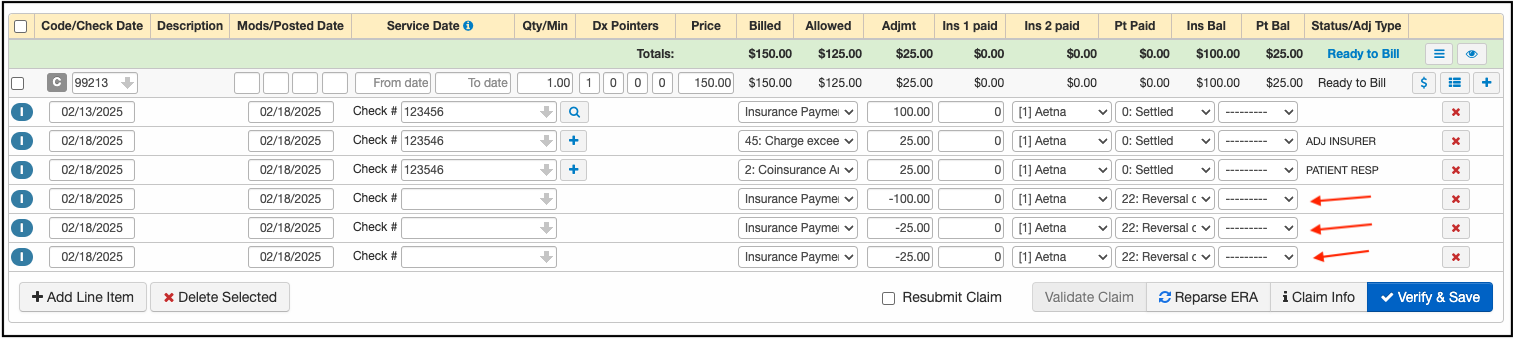
- Once entered press Verify & Save.
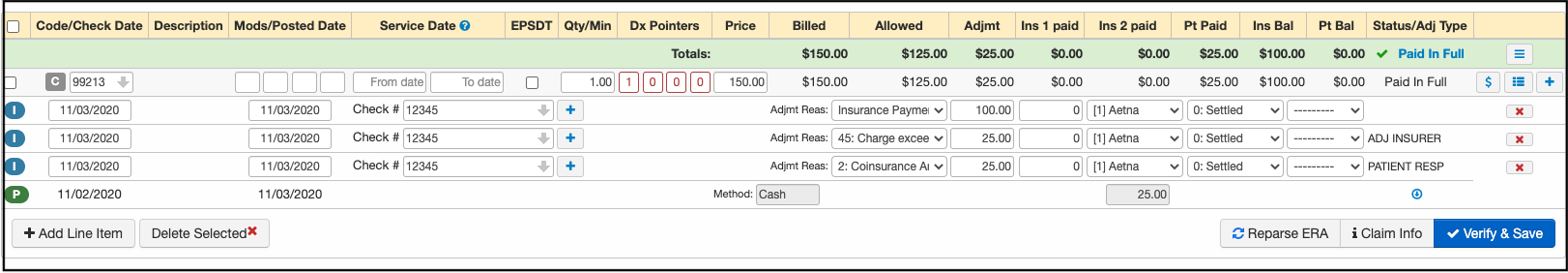
Now, the insurance balance will show as outstanding and you can proceed with either appealing the retraction, billing the patient, or adjusting the balance, depending on the situation.
Please be sure to add the EOB/Correspondence to your Remittance Report section so that the image is available on demand within the appointment. For instructions on how to attach an EOB, please see this article.