When a payer has issued an authorization number for specific services, the information can be entered directly into the patient's account. This ensures that the authorization details are automatically populated on the appropriate claim form—whether utilizing the CMS-1500 (formerly HCFA-1500) or UB-04 format— streamlining the billing process and reducing the risk of claim denials due to missing authorization information. This workflow enhances efficiency while maintaining compliance with payer requirements and facilitating accurate claims submission.
- In a patient's chart, select the Demographics tab and then Authorizations.

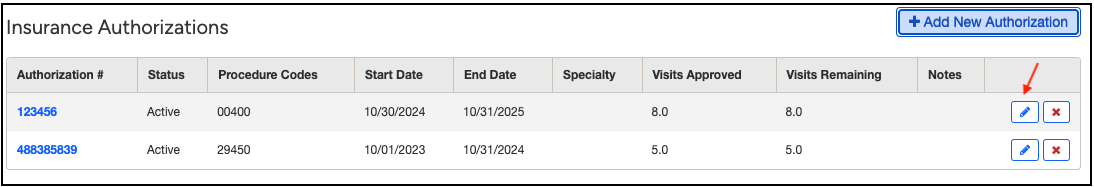
- Select Add New Authorization.

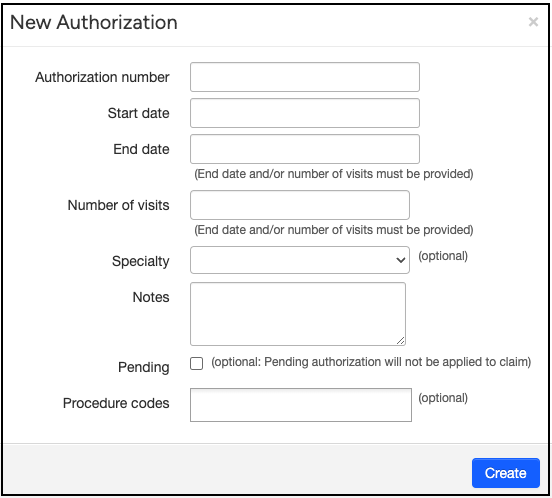
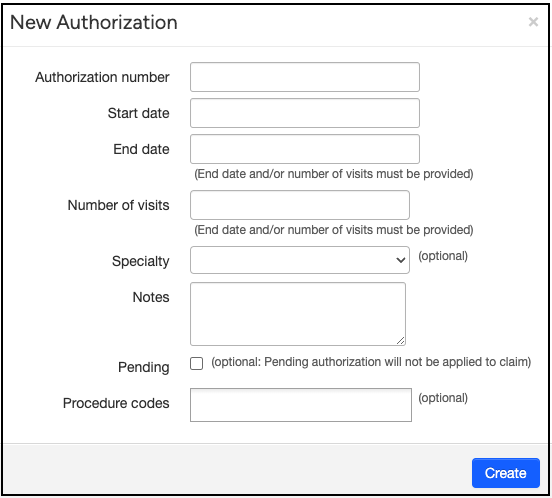
- Fill in all of the information you have available, including the authorization number, effective dates, and any notes that you may want to include.
- You can add additional information by returning to the Authorizations section of the patient's chart and selecting
 .
.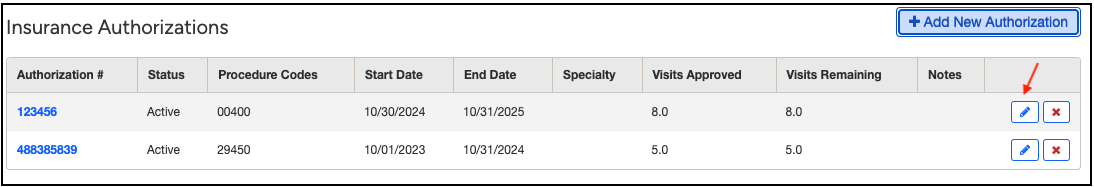
- Any authorizations entered and listed as active (and not checked as "pending") will automatically print on either the CMS-1500 form or UB04 when the date of service on the claim matches the start/end date or procedure code listed.
- If you are billing on a UB04, the authorization number can also be entered on the patient's claim by going to Billing > Live Claims Feed > Inside the patient's claim > right side of the screen > Insurance tab.

As an authorization nears expiration—either due to the approved number of visits being used or the end date approaching—a warning label will appear on the patient’s account to alert you in advance.