Customers utilizing eProvider Solutions (ePS) can now validate claims on demand. This ability will identify any errors quickly and allow for correction before the claim is submitted to the clearinghouse for processing.
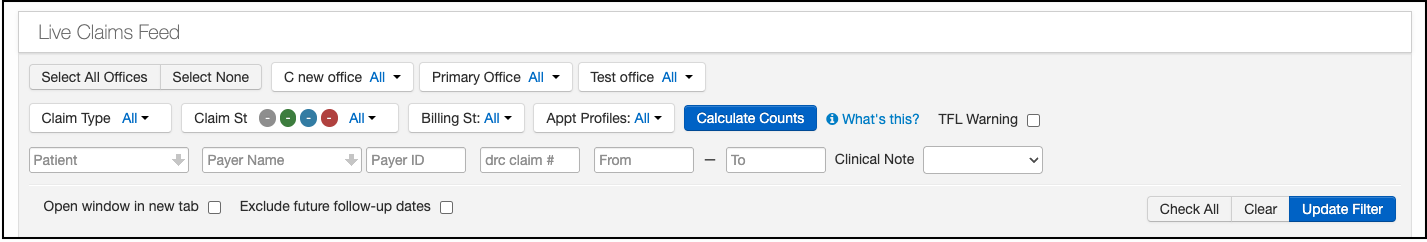
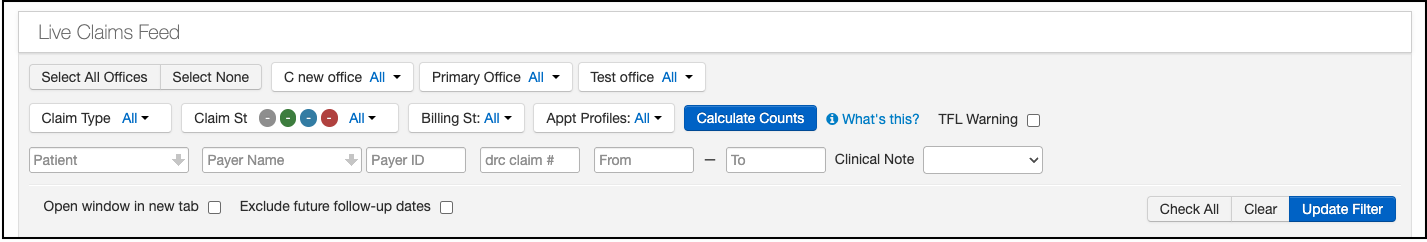
- Navigate to Billing > Live Claims Feed
- Pull up the claim needing validation by entering the patient's name, billing status, or date of service.
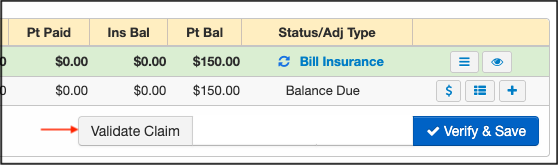
- Scroll down to the area where the charges appear.
- Press Validate Claim.
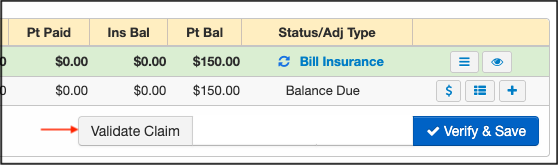
- Any upfront errors found will be notated so they can be adjusted prior to submission.
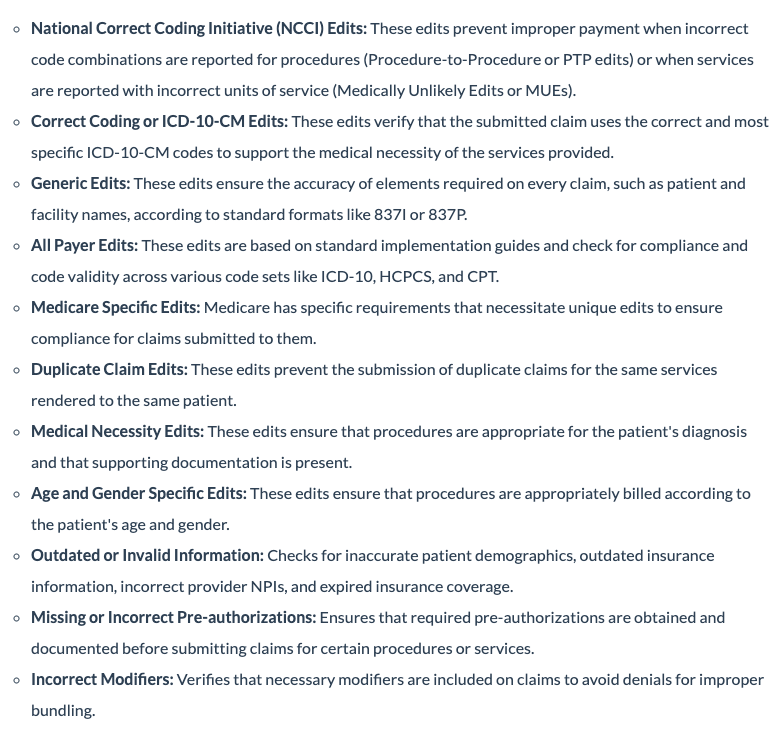
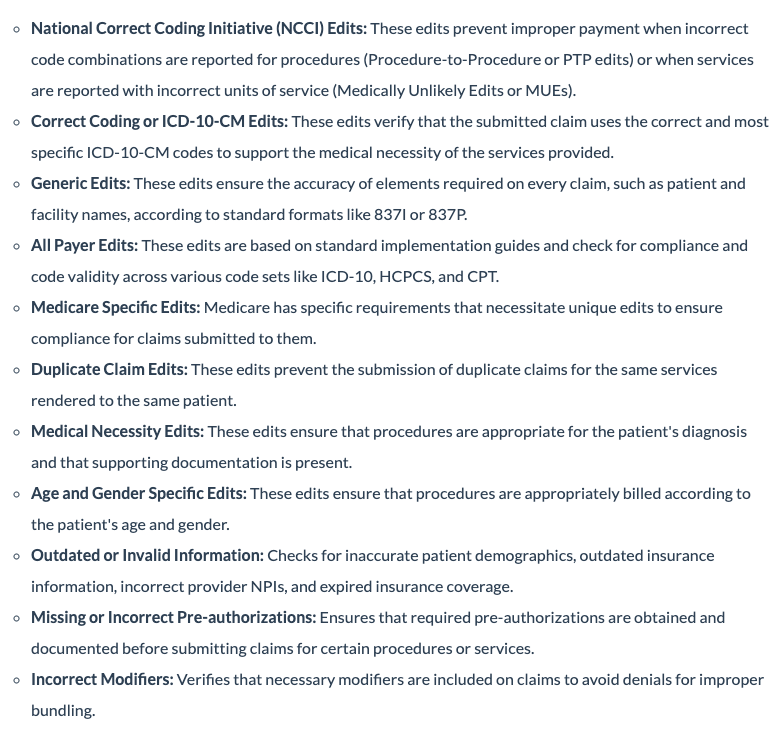
- The following list is of common, but not all-inclusive, upfront edits. Please note, upfront edits can be specific to a payer and may not be included in this list.
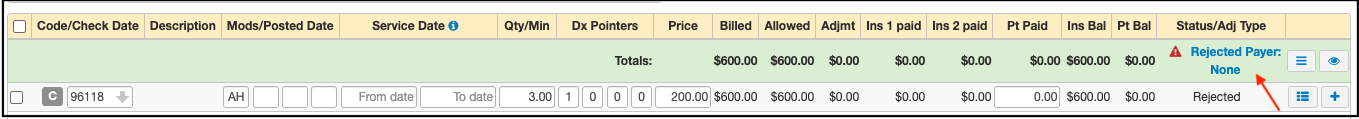
- If the claim does not successfully pass all of the upfront edits, a message will appear in the patient's claim under Status/Adj Type.
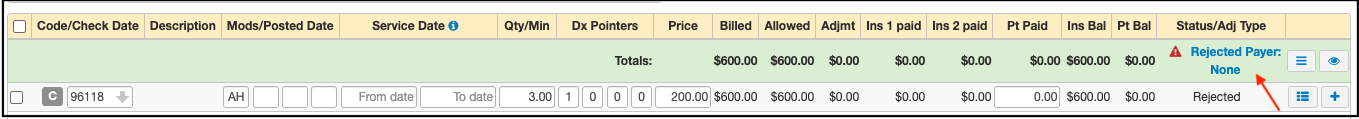
- Depending on how the information is returned to DrChrono, the abbreviated reason may or may not tell you what the exact error is. More information about the rejection can be found by pressing on the blue words "Rejected Payer: None" (for the example above).
- A window will open with additional information regarding the rejection. Once that is known, the information on the claim can be updated and then resubmitted to the clearinghouse.