If you are utilizing eProvider Solutions (ePS) as your clearinghouse, your claims will now have a pre-scrubbing before being submitted to the payer. This scrubbing will alert you to any missing information or errors in the claim in real-time so they can be corrected without waiting for the actual submission.
Here is how it works:
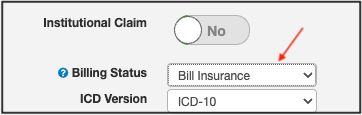
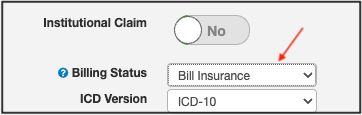
- When you update a claim status to any of the submission statuses (Bill Insurance, Bill Secondary Insurance, Resubmit Claims), the DrChrono system will scrub the claim using the same parameters that ePS uses.
- If any issues are found, the status of the claim will update to "Missing Information: [Reason]". You will be able to see this real-time information under the Claim Status tab in your Live Claims Feed.

If you open the claim, you will see the exact reason for the rejection so it can be addressed before the claim submission to the clearinghouse and payer. Having this information quickly will increase your clean claims rate and help speed up your claims reaching the payer so they can be processed promptly.