You can send a corrected claim by following the below steps to all payers except Medicare (Medicare does not accept corrected claims electronically).
To submit a corrected claim to Medicare, make the correction, and resubmit it as a regular claim (Claim Type is Default) and Medicare will process it.
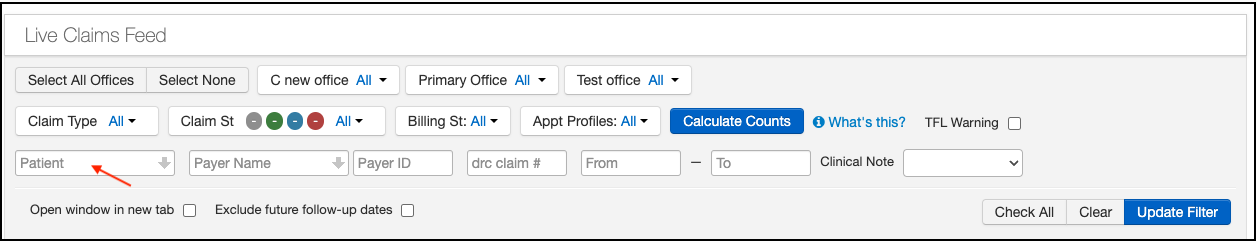
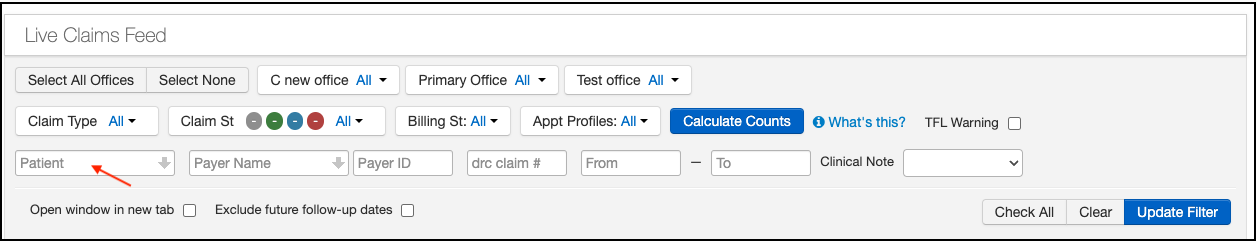
- Hover over the Billing tab and select Live Claims Feed.
- Search for the patient and select the from the drop-down.
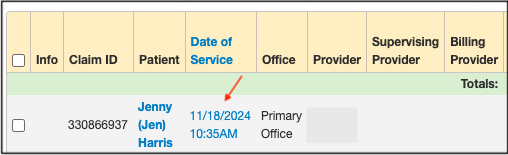
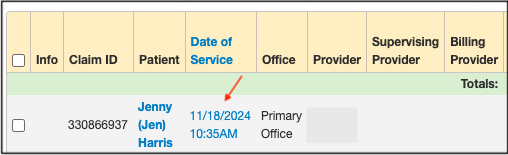
- Press on the appointment date, and it will take you to the Billing Detail screen.
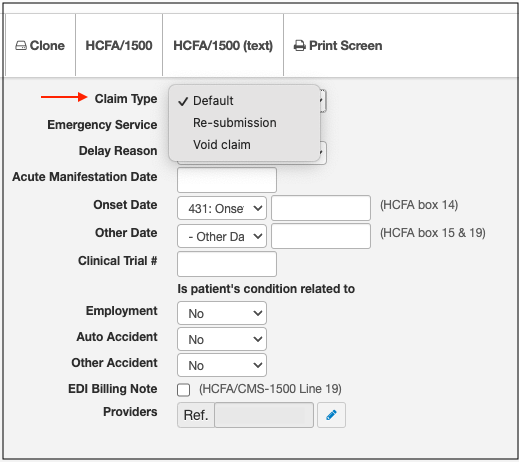
- Press on the Claim Type field and select Re-submission from the drop-down. (Please note, that Medicare does not accept re-submitted claims. If you need to resend a claim to Medicare, please use the default option to avoid rejection.)
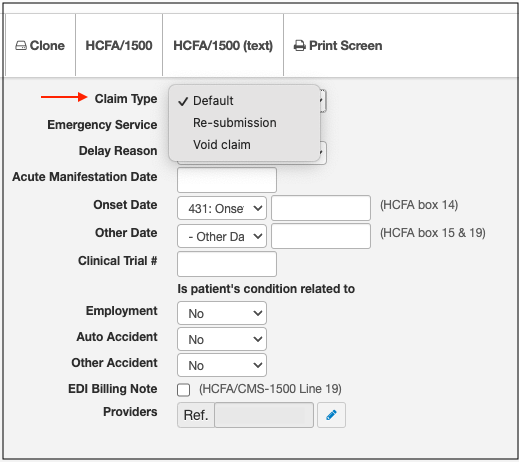
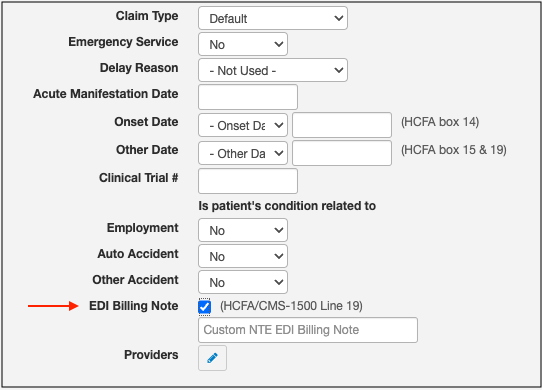
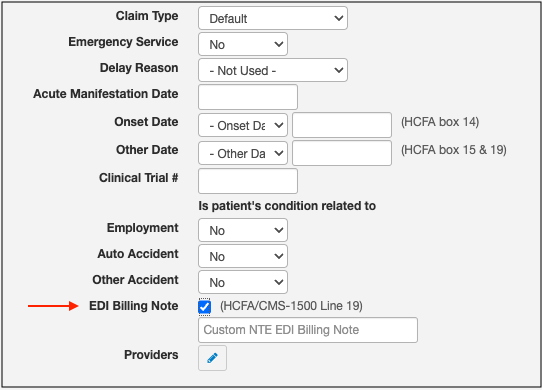
- Check the box EDI Billing Note and enter the reason for the resubmission. (Ex: Resubmitting the CPT Code: 99213).
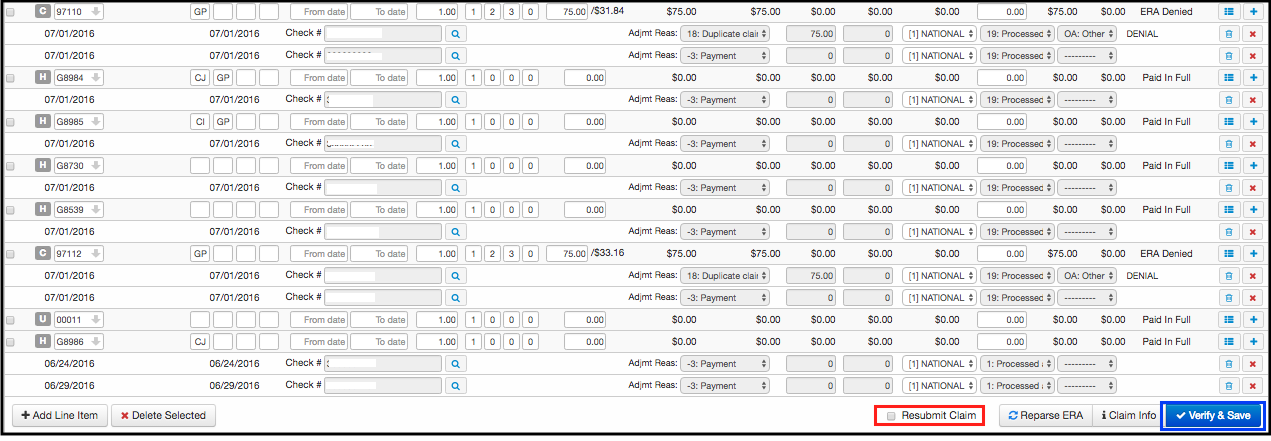
- Please make sure you check the box Re-submit Claim.
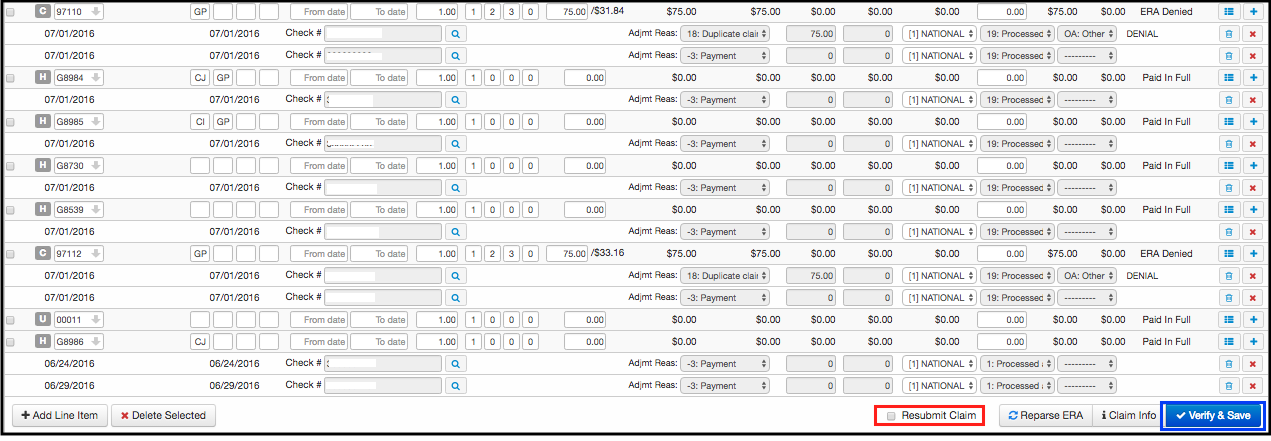
- Select the billing status as **Bill insurance** for primary and **bill secondary** for secondary claims and press Verify & Save.
Please note you will not be able to bill only the partial code alone that was denied.