**** Please note, if you submit any request other than real-time eligibility (Claims and/or ERA) you could potentially impact ALL of your claim submissions ****
For any questions, please reach out to support.
Here is how you can enroll with eProvider Solutions (ePS) for eligibility checks (RTE) only.
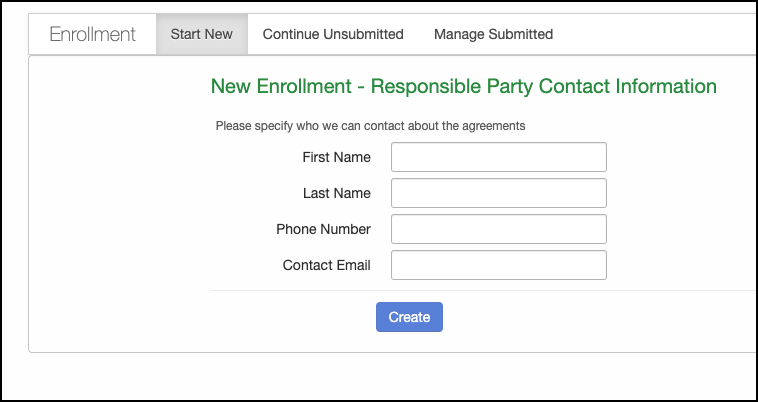
- Navigate to Billing > Enrollment.
- The screen that appears will begin the process by entering the responsible party's contact information.
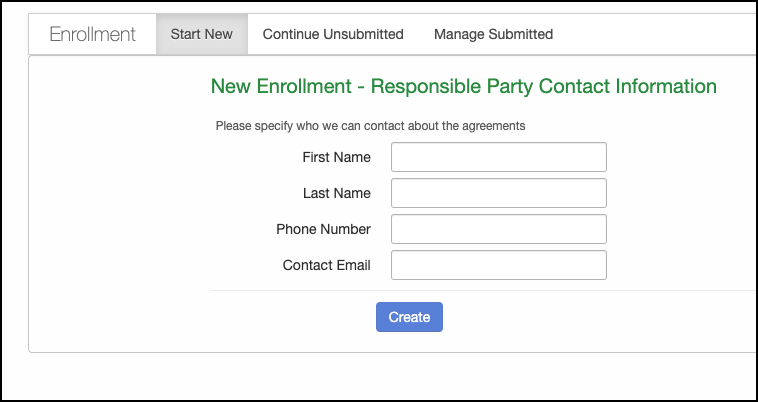
- Once it is filled in, press Create.
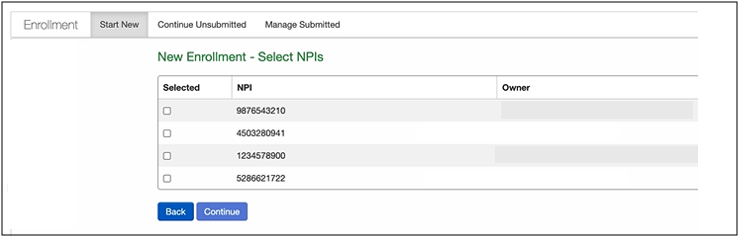
- The next screen will ask you which NPI you are submitting the request under (if you have multiple). Press in the box to the left of the NPI to select. The system will pull demographic information associated with the NPI for verification.
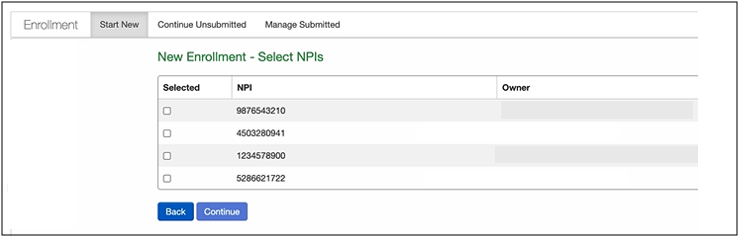
- Once selected and the information verified, press Continue.
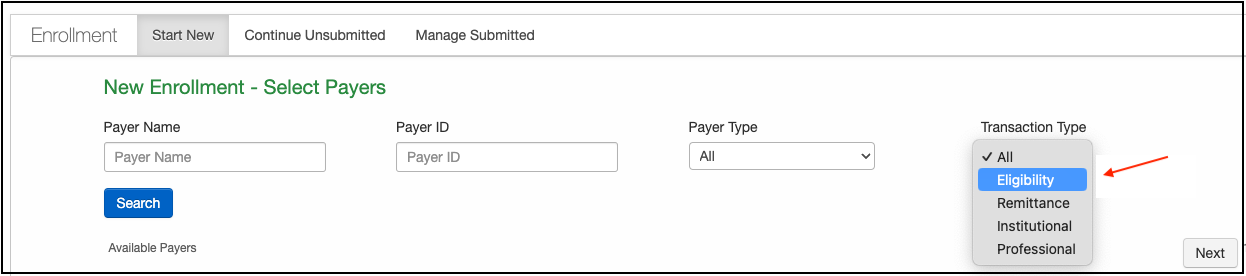
- The following screen is where you will request eligibility enrollment with your payers.
- You will first want to select "Eligibility" under the Transaction Type drop-down.
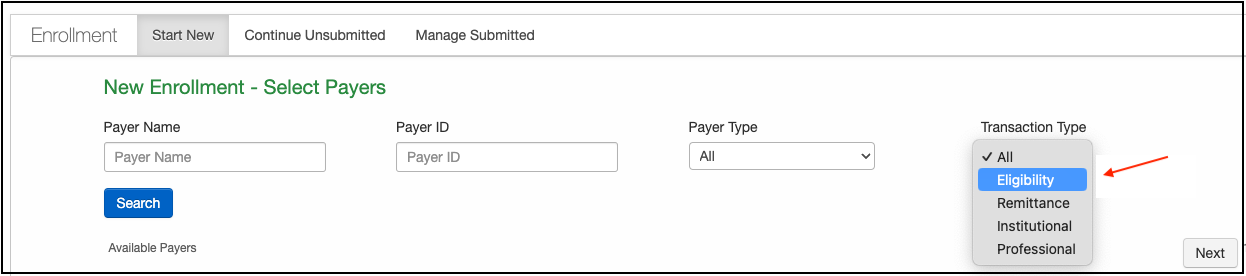
- You will first want to select "Eligibility" under the Transaction Type drop-down.
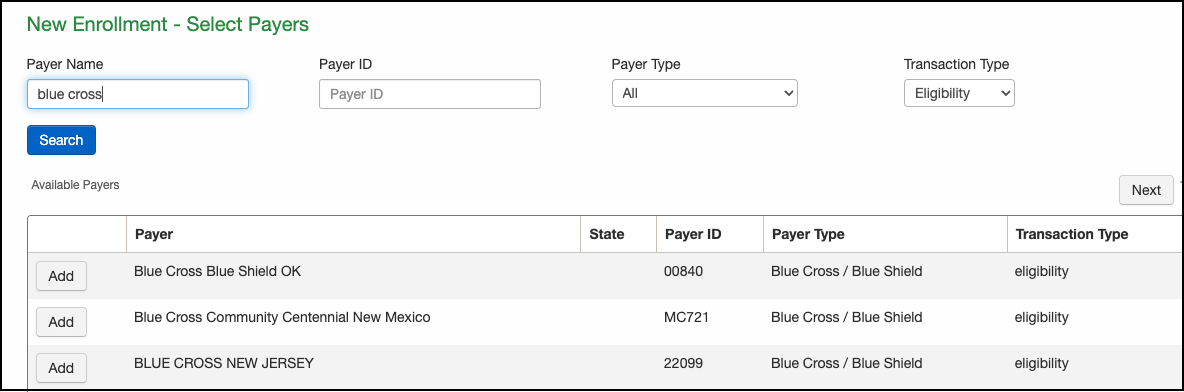
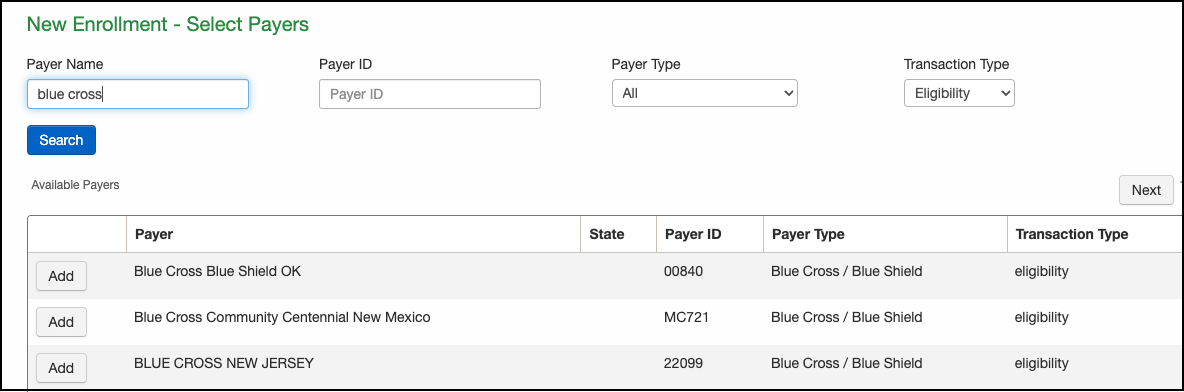
- From here, you can select your payers by entering the payer name or payer ID, if known.
- Press Search after you have entered the information. The payers that offer eligibility that meet your search criteria will appear. To select a payer, press Add on the screen's left.
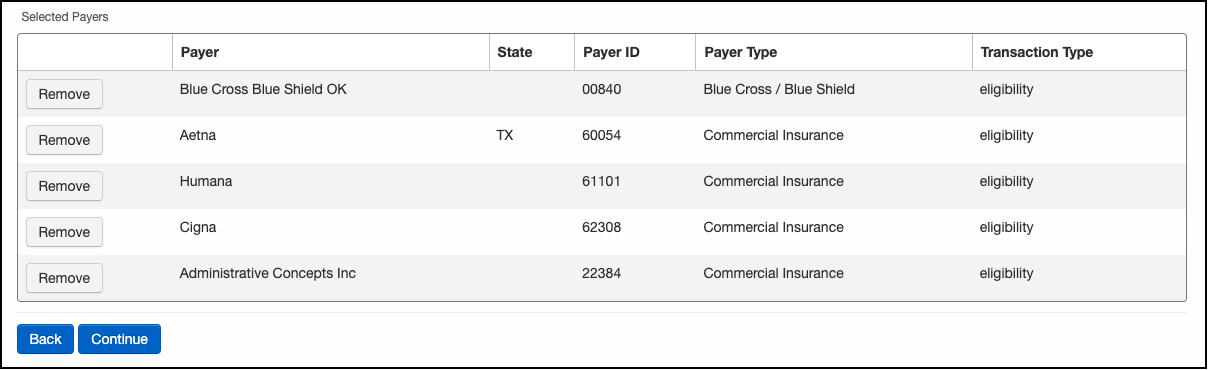
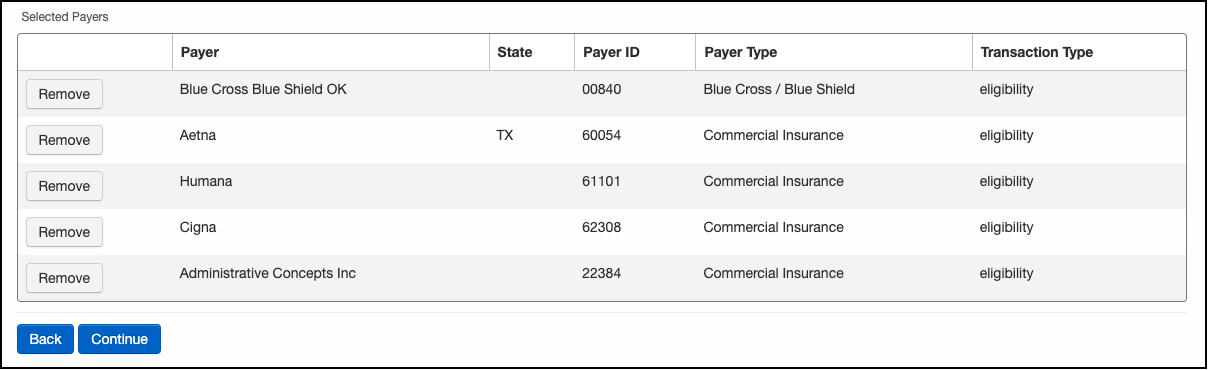
- Once your payers have been selected, they will appear in a list at the bottom of the screen. You can use this list to ensure that you have selected all of the payers you need, as well as remove any that you do not need. When you are satisfied with the list, press Continue.
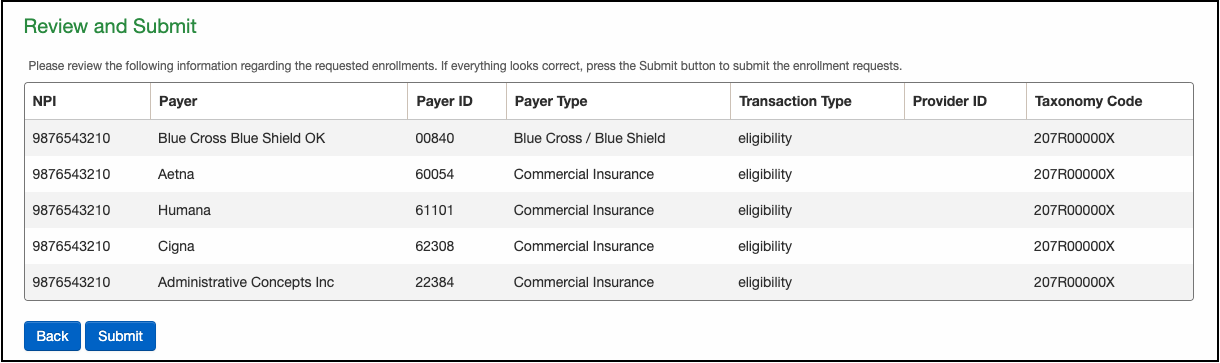
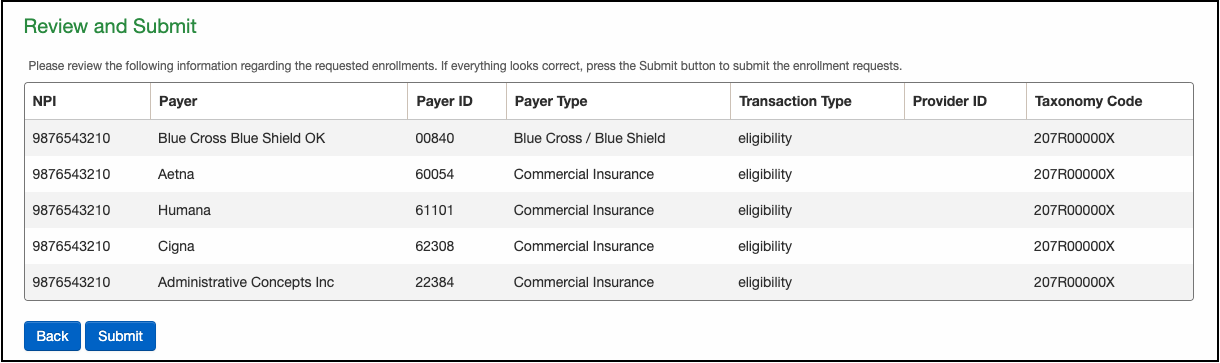
- The next and last screen you will see before the requests are submitted is titled Review and Submit. If all looks good to you, press Submit. The requests will route through ePS to the payer.
- To check on the status of your submitted request, you can do so under the Managed Submitted tab. It will list all of your requests and the current state under the Status column.