DrChrono uses statuses on appointments/claims to know, at a glance, where claims are in the RCM process. These statuses are in the Live Claims Feed.
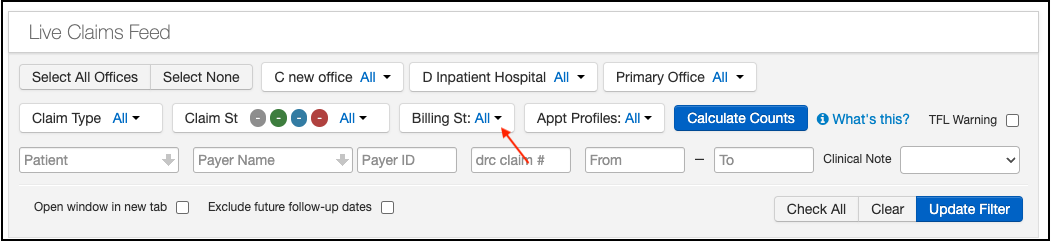
- Navigate to Billing > Live Claims Feed.
- Once you select your date range, press the blue Calculate Counts button, the system will fill in the colored bubbles to let you see a count of how many claims are in that particular status at that time.

Please note, that these figures can and do change during the day as claims are submitted, patient payments posted and ERAs are received.
Your DrChrono account will have many common pre-populated billing statuses listed. Depending on your workflow, you may or may not use all of these. The ones below the gray line below (under the shortlist that ends with "other"), can be rearranged, or hidden from view if you would like.
Here is a link to an article showing you how to create additional or custom billing statuses for your practice.
Some of the listed statuses are utilized when you are using DrChrono RCM services, however, if you are doing your billing, they can be used by your billing staff as well. Your RCM Account Manager and Billing Manager will assist in talking through your workflow and which statuses the office should monitor.

- Paid In Full - There is no balance due from either the patient or the payer
- Settled - The claim has been settled. No further attempts to collect will occur
- Balance Due - There is a balance due from the patient
- Internal Review - This status can be used for any type of internal review/audit situation
- Scrubbing Error - This status is a placeholder for a future enhancement
- Other - Could include statuses such as not submitted, payer acknowledged, rejected or ERA denied
- Attention to Biller - Used to alert the biller that there is an action that needs to be taken on the claim
- Specialist Review - Used when a claim is referred to a senior biller/supervisor for review
- Pending Info Practice - Used when input from the office is needed to move forward with the claim
- Coding Completed - Used when the coding team has completed their review of the clinical note and has added the ICD-10, CPT, HCPCS, and/or custom codes to the claim
- Coding Clarified - Used when the provider has given additional details regarding the clinical visit so the claim can be coded appropriately
- Coding Clarification - Used when the coding team needs additional clinical details to code the claim appropriately
- Patient Contact - Used when a reach out to the patient is needed
- Payer Contact - Used when a reach out to the payer is needed
- Internal Coding Review - Used when a senior coder/supervisor reviews the coding. Also used for internal auditing purposes
- Analyst Review - Used when a claim is referred to a senior biller/supervisor for review
- In Process w Payer - Used when the billing team has received information from a payer that a claim has been received and is being processed. This status is usually used when no ERA "payer acknowledged" was received
- Chrono Appeal - Used when DrChrono is appealing a claim denial
- Faxed/Mailed Claim or Appeal - Used when DrChrono has sent the appeal to the payer and is awaiting a response
- Paid Not Posted - Used when the billing team receives information from the payer that a claim has been processed and paid but we have not yet received the ERA or the EOB to post
- Chrono Audit - Used when internal management staff is auditing a claim to ensure correct coding and billing
- Ready to Bill - Used to signal the biller that a claim is ready to be billed to a payer
- Voicemail Follow-Up - Used when the biller has left a voicemail for either the patient and/or payer and is awaiting a response. Claims will be followed up on if no response is received.
- Enrollment Pending - Example of a custom billing status. Used when credentialing with a payer is complete and EDI enrollment is pending with the clearinghouse to submit claims.