If your claim is denied for timely filing, you can appeal the claim with the proof of timely filing if it was filed within the payer's established guidelines.
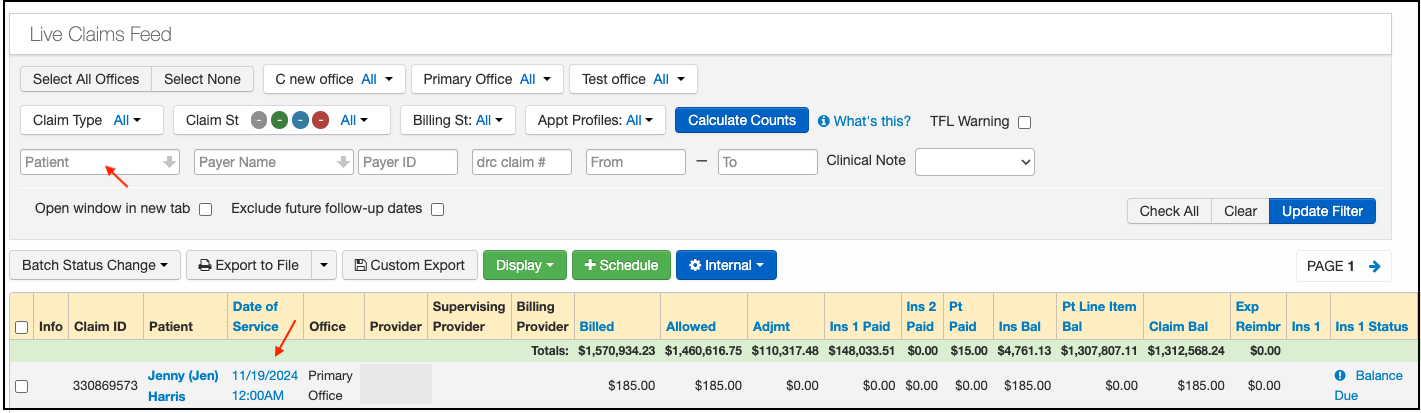
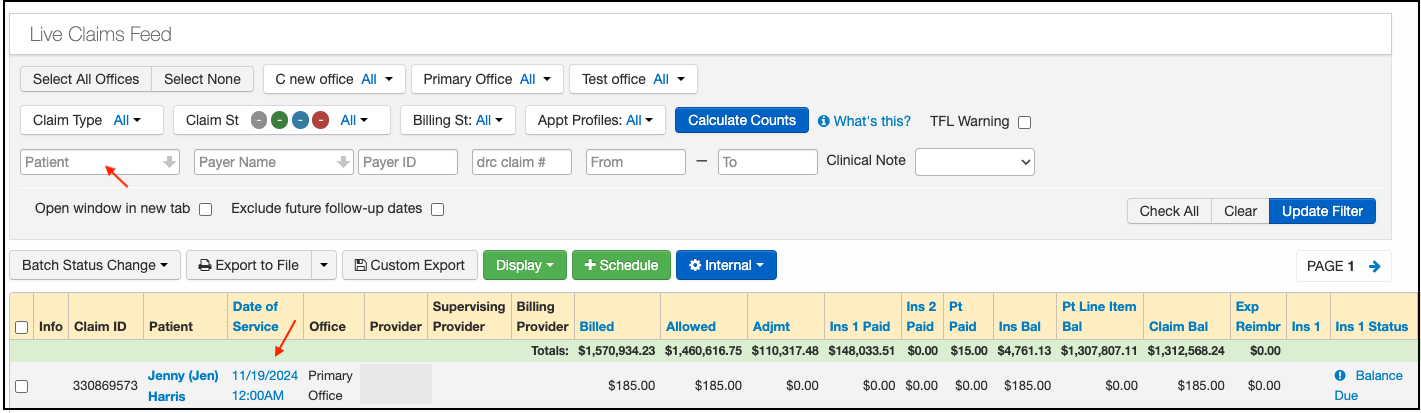
- Hover over the Billing tab and select Live Claims Feed.
- Filter by the patient name or Chart ID, then click on the visit date. This will direct you to the Billing Detail screen.
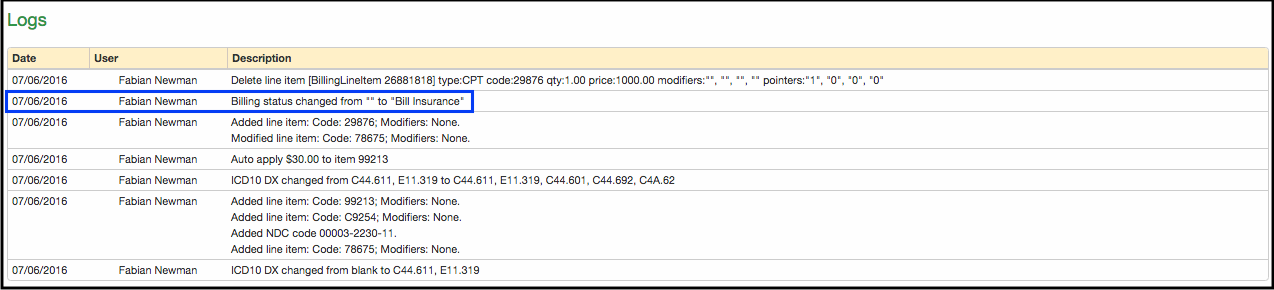
- You will find the Log section if you scroll down under the CPT/HCPCS codes. Listed in this log will be the date/time/user of when the claim was set to the Bill Insurance status. The claim would have been sent on that date to the payer. This is your proof that the claim was submitted within the payer's timely filing limit.
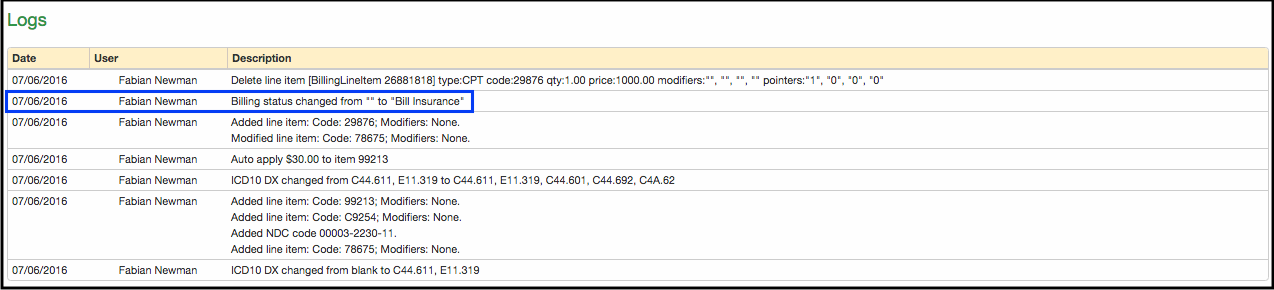
- You can also include the date/time of the "payer acknowledged" status. That status comes directly from a 277 file sent by the payer acknowledging receipt of the claim.
- Press Print Screen at the top right corner to print the entire screen, including the log. This can be submitted with your appeal.